Introduction
Falls with major injury represent one of the most challenging clinical events in long-term care. Not only do they cause significant harm to residents, but they also directly impact your facility's quality measures and CMS star ratings. With the October 2025 release of the updated RAI Manual, CMS has clarified definitions around falls and fall-related injuries—and these changes affect how you document, code, and prevent these incidents. Whether you're struggling to improve your quality measures or simply want to ensure your team is coding correctly, understanding the new guidance is essential. In this post, I'll walk you through the updated definitions, explain how falls with major injury impact your quality measures, and share practical prevention strategies to help protect your residents and strengthen your facility's performance.
Clear, New Definitions
Per the Long-Term Care Facility Resident Assessment Instrument (RAI) 3.0 User’s Manual, Version 1.20.1, released in October 2025, the definitions for fall and fall with major injury have been updated. (Per CMS process, anything in red is a new addition to this version of the manual.)
A fall is defined as:
- Unintentional change in position coming to rest on the ground, floor, or onto the next lower surface (e.g., onto a bed, chair, or bedside mat)
- The result of an overwhelming external force (e.g., a resident pushes another resident)
- An intercepted fall occurs when the resident would have fallen if they had not caught themself or had not been intercepted by another person. This is still considered a fall.
CMS’ additional coding tips:
- The fall may be witnessed, reported by the resident or an observer or identified when a resident is found on the floor or ground.
- Falls include any fall, no matter whether it occurred at home, while out in the community, in an acute hospital, or a nursing home.
- CMS understands that challenging a resident’s balance and training them to recover from a loss of balance is an intentional therapeutic intervention and does not consider anticipated losses of balance that occur during supervised therapeutic interventions as intercepted falls. However, if there is a loss of balance during supervised therapeutic interventions and the resident comes to rest on the ground, floor, or next lower surface despite the clinician’s effort to intercept the loss of balance, it is considered a fall.
A fall with major injury includes, but is not limited to, traumatic bone fractures, joint dislocations/subluxations, internal organ injuries, amputations, spinal cord injuries, head injuries, and crush injuries.
CMS’ additional coding tips:
- If the level of injury directly related to a fall that occurred during the look-back period is identified after the ARD and is at a different injury level than what was originally coded on an assessment that was submitted to the Internet Quality Improvement and Evaluation System (iQIES), the assessment must be modified to update the level of injury that occurred with that fall.
- Fractures confirmed to be pathologic (vs. traumatic) are not considered a major injury resulting from a fall.
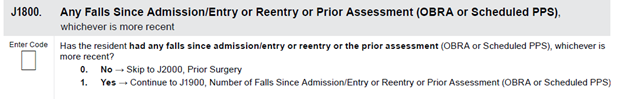
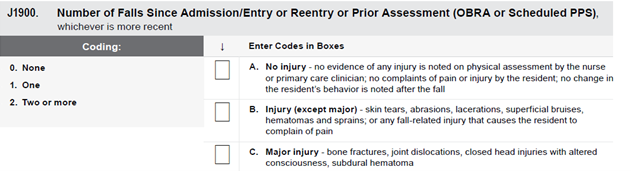
Fall with Major Injury: MDS Coding
The Minimum Data Set (MDS) is a standardized assessment used in Medicare and Medicaid- certified nursing homes to collect demographic and clinical information about residents.
How Falls with Major Injury Impact Quality Measures (QMs)
Just like so many areas of the MDS, coding of fall with major injury will affect nursing homes quality measures. Let’s see how it is calculated:
Numerator:
-
A resident is counted in this measure if any of their assessments during the look-back period indicate a fall with major injury.
-
Residents are not counted if none of their assessments during the review period recorded whether they had a fall with major injury.
-
A resident is included in the numerator if any look-back scan assessment indicates a fall with major injury by coding of J1900C = 1 or 2.
Denominator:
-
All long-stay residents with one or more qualifying assessments in the look-back scan.
-
Long-stay residents are defined as being in the facility greater than 101 days.
Look-back details:
-
The look-back scan includes the target assessment and all qualifying earlier assessments within the resident’s episode.
-
Assessments are included if:
-
They are within the same episode
-
They have a qualifying Reason for Assessment (RFA)
-
Their target date is on or before the target assessment’s date
-
Their target date is no more than 275 days before the target assessment
-
How to Prevent Deficiencies: Critical Element Pathways and Appendix PP
Per F Tag 689, the intent of this requirement is to ensure the facility provides an environment that is free from accident hazards over which the facility has control and provides supervision and assistive devices to each resident to prevent avoidable accidents. This includes:
- Identifying hazards and risks
- Evaluating and analyzing hazards and risks
- Implementing interventions to reduce hazards and risks
- Monitoring for effectiveness and modifying interventions when necessary
Per the RAI Manual, effective fall prevention and management require a comprehensive approach thru risk identification and intervention strategies.
Risk Identification: Recognizing residents at high risk for falls is essential. This includes evaluating both intrinsic factors (e.g., functional decline, delirium, adverse drug reactions, dehydration, infections) and extrinsic factors (e.g., medication side effects, use of appliances or restraints, environmental hazards).
Intervention Strategies: A fall should prompt a thorough evaluation of a resident’s needs, including rehabilitation services, ambulation aids, environmental modifications, and increased monitoring (e.g., toileting assistance to prevent incontinence-related falls). Falls may also signal the onset of serious medical conditions and should be treated as a sentinel event requiring immediate attention and reassessment of the care plan.
Working through the CMS Critical Elements Pathways (CMS 20127 – Accidents) can help facilities ensure that they have appropriate processes in place to prevent accidents and injuries.
5 Areas of Fall Risks from a Clinical Perspective
- Medication can affect balance, cognition, or blood pressure, increasing fall risk.
-
Orthostatic hypotension, a sudden drop in blood pressure when standing, may cause dizziness and instability.
-
Vision impairments can make it difficult to detect hazards in the environment.
-
Mobility limitations, such as muscle weakness or poor coordination, reduce a person’s ability to move safely and increase fall risk.
-
Unsafe behaviors, including rushing, not using assistive devices, or ignoring safety protocols, can significantly heighten the chance of falling.
Interim Plan of Care Post-Fall
- Close observation and increased supervision
- Frequent orientation to room, bathroom, and facility
- Medication review
- Use of safe footwear
- Staff assistance to toilet or bedside commode
- Use of monitoring or sensor devices
- Use of pressure, position, or other alarms
- Use of protective clothing/devices
Conclusion
Falls with major injury are more than isolated incidents - they are sentinel events that reflect the quality of care and safety within long-term care facilities. With updated definitions and coding guidance from CMS, it is critical for providers to understand how these events impact quality measures and regulatory compliance. Accurate documentation, proactive risk identification, and timely interventions are essential to prevent deficiencies and improve resident outcomes. By leveraging tools like the Critical Element Pathways and Appendix PP, facilities can strengthen their fall prevention strategies and ensure a safer environment for all residents. Ultimately, a comprehensive, resident-centered approach to fall management not only supports regulatory standards but also promotes dignity, safety, and quality of life.
Download Our Fall With Major Injury Quality Measure Reference Guide
 Accurately identifying and coding falls with major injury is essential for quality reporting and Five-Star performance. To make this complex CMS measure easier for your team, we’ve created two practical tools: a detailed Resource Sheet and a quick-reference Flowchart. Together, they break down Measure 2-12: Falls with Major Injury – Long-Stay Residents into clear, actionable guidance your staff can use right away.
Accurately identifying and coding falls with major injury is essential for quality reporting and Five-Star performance. To make this complex CMS measure easier for your team, we’ve created two practical tools: a detailed Resource Sheet and a quick-reference Flowchart. Together, they break down Measure 2-12: Falls with Major Injury – Long-Stay Residents into clear, actionable guidance your staff can use right away.
These essential resources include:
-
A plain-language overview of what counts as a major injury (fractures, dislocations, internal organ injuries, head injuries, and more)
-
A clear explanation of how the measure is calculated—including numerator, denominator, and exclusions
-
Step-by-step logic for the look-back scan used to identify qualifying assessments
-
A breakdown of MDS Item J1900C and its coding values
-
Common coding scenarios with real examples (Residents A–D)
-
Easy-to-follow flowcharts to help staff quickly determine inclusion or exclusion
-
Practical implementation notes, including long-stay criteria, episode rules, and Five-Star implications
These resources make it simple for your team to understand exactly how CMS evaluates falls with major injury—helping you improve accuracy, reduce errors, and strengthen your facility’s quality measure performance. Perfect for onboarding, training refreshers, and daily quality assurance.
Additional Resources
- CMS Quality Measures User Manual
- CMS MDS RAI Manual
- CMS Critical Elements Pathways
- CMS Appendix PP
- Post-Acute and Long-Term Care Medical Association. Falls and Fall Risk Clinical Practice Guideline. Columbia, MD: PALTmed 2011.

Struggling with Your CMS 5-Star Rating?
.png?width=248&height=192&name=A%20Proven%20Program%20for%20Nursing%20Home%20Quality%20Improvement%20(17).png)
Discover how our 5 Steps to 5 Stars program has helped nursing homes transform from struggling to top-performing.



.png?width=300&name=Nursing%20Home%20Insights%20Blog%20Featured%20+%20Social%20Images%20-%20Hubspot%20&%20Insta%20(25).png)
